Dhealthwellness.com – Whether you are considering getting inner ear surgery or have already had it, there are a number of important factors that you will need to consider. These factors are the surgeon’s experience, the type of procedure performed, and the outcome of the operation.
Performing a Ventral Approach for Inner Ear Surgery
Performing a ventral approach to inner ear surgery is less invasive than dorsal approaches. However, a number of surgical complications are possible and some of them may require re-intervention. One common complication is hemorrhage. Gelfoam can be placed over the site of the hemorrhage to aid in the evacuation. Bishop-Harmon forceps can also be used to help evacuate the blood.
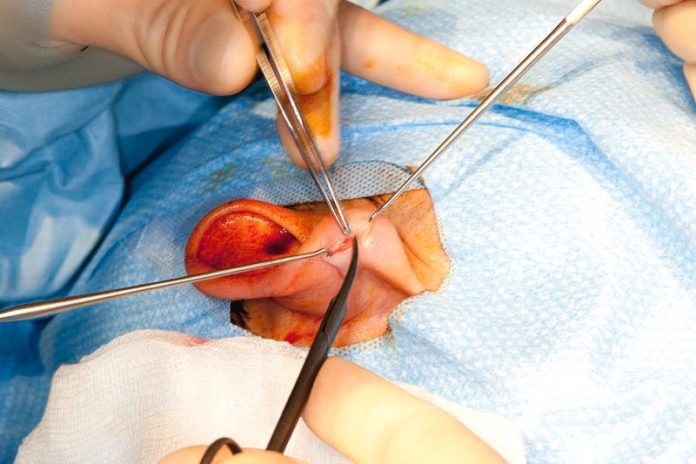
In the ventral approach, the bulla is exposed through a small incision in the neck. This allows access to the tympanic cavity and the osseous ear canal. The tympanic membrane is then assessed for signs of otitis media. If any are present, antibiotics are prescribed. A ventral midline skin incision is made from the larynx to the manubrium of the sternum. The external occipital protuberance (EOP) is also shaved. Swabs are then taken for sensitivity testing and bacterial culture.

Compared with the conventional approach, a postauricular approach for inner ear surgery is faster and easier. This is because the incision is made behind the outer ear crease. It also provides the surgeon with an excellent view of the eardrum. This enables the preservation of the GAN and LON. This approach is especially suitable for patients with small ear canals. Consequently, the use of this technique has become more common in the past few years. It is a well-known fact that this approach has a 90-98% success rate in closing tympanic membrane perforations.
The Ideal Route for Minimally Invasive Ear Surgery
During the procedure, the facial nerve is protected from injury by a retractor. This prevents the nerve from being sliced during the surgery. Several studies have shown that the transcanal approach for inner ear surgery can enhance drug delivery into the middle ear. In addition, this approach does not involve structural damage to the inner ear, which is common during conventional ear surgery. The benefits of this method are that there is no skin incision, minimal recovery time, and no loss of hair. This makes it an ideal route for minimally invasive ear surgery. It also offers greater visibility during cholesteatoma resection. It may reduce the risk of residual cholesteatoma.
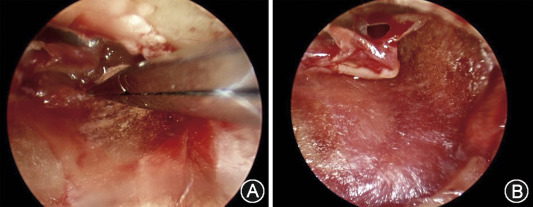
To evaluate the efficacy of this approach, a transcanal USMB (USMB) exposure was simulated. A tympanic membrane from guinea pigs was placed in a chamber and covered on top with tissue-mimicking agarose phantoms. A fluorescent drug was then delivered into the middle ear cavity via a transtympanic injection. The fluorescence intensity of the biotin-FITC was higher in the USM group than in the RWS group.
Perilymphatic Fistula Occurs When There is a Tear in the Membrane
Perilymphatic fistula Unlike other conditions that can cause fistulas, a perilymphatic fistula occurs when there is a tear in a membrane that covers an oval or round window in the middle ear. While some cases heal on their own, others need surgical repair. This condition affects the pressure in the middle ear. It is also known to affect hearing, but how much it affects hearing depends on several factors.
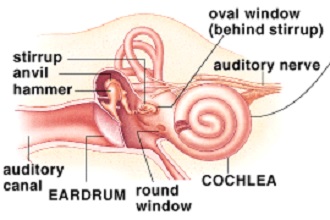
In most cases, a perilymphatic fistula develops after a rapid increase or decrease in the pressure within the inner ear. However, it can also occur after a head injury or barotrauma. The symptoms of a perilymphatic fistula include imbalance, dizziness, vomiting, nausea, and ringing in the ears. If you experience any of these symptoms, you should seek medical attention immediately. Despite the fact that surgical stress is associated with potential short and long-term consequences, little is known about the inflammatory response after abdominal operations. Knowing the specific cytokine and WBC count subgroups, and their peak response, may help minimize the negative effects of abdominal surgery. Identifying the relevant factors can also help to determine the magnitude of the inflammatory response to abdominal surgery.
Reference :